
Introduction:
The second month of pregnancy (the subsequent month of the first month) marks an exciting and transformative time, as your body begins to undergo significant changes to support the development of your baby. This early stage of pregnancy is often filled with a mix of emotions—from joy and anticipation to uncertainty and curiosity. While many physical changes are happening internally, they may not yet be visible on the outside. However, the signs and symptoms you experience during this month are essential indicators of your body’s preparation for the months ahead.
During the second month, it’s common to experience early pregnancy symptoms like nausea, fatigue, and mild cramping. These changes, although sometimes uncomfortable, are typical as your body adjusts to its new role. Understanding what to expect and how to care for yourself during this time can help you feel more in control and at ease with the process.
This guide will provide you with valuable insights into what happens during the second month of pregnancy, address common concerns, and offer practical advice on self-care and planning for the months ahead. Whether this is your first pregnancy or you’ve been through it before, having a clear understanding of what’s happening can make this journey more comfortable and reassuring.
Contents:
- Understanding the Second Month of Pregnancy
- How Physical and Emotional Changes Occur
- How Baby’s Development Takes Place in the Second Month (Formation of Brain, Heart, and Spinal Cord)
- How Prenatal Care Can Be Ensured (First Ultrasound, Blood Tests, etc.)
- What shall be the Proper Nutrition and Diet
- Lifestyle Adjustment Requirements
- Common Concerns and Questions
- Moving Ahead to the Next Step (The Third Month of Pregnancy)
- The Final Thoughts
Understanding the Second Month of Pregnancy:
The second month is often when many women start to recognize the early signs of pregnancy, such as morning sickness and fatigue. It’s a period of rapid growth for the embryo, with essential organs and systems beginning to form. This month lays the groundwork for the baby’s overall development, making it a critical phase in the pregnancy. The changes occurring now will impact both the mother’s health and the baby’s well-being throughout the entire pregnancy.
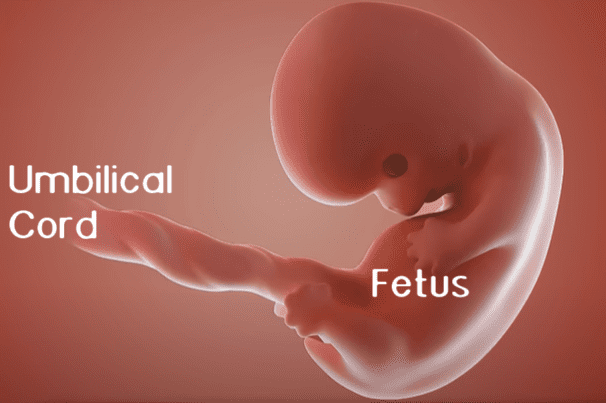
The second month of pregnancy spans from weeks 5 to 8. During this time, the embryo grows from a tiny cluster of cells (of poppy seed size) into a more defined form, beginning to resemble a human. By the end of the eighth week, the baby is typically about the size of a raspberry ((1.2 to 2 centimeters in diameter) and is starting to develop the basic structures of the brain, heart, and limbs. By the end of the 8th week of pregnancy, the embryo transitions into what is medically termed a fetus. For the mother, this is often the period when pregnancy symptoms become more pronounced, leading to the realization that a new life is taking shape.
Source: American Pregnancy Association
How Physical and Emotional Changes Occur:
A. Physical Changes:
1. Morning Sickness:
One of the most common symptoms during the second month, morning sickness usually manifests as nausea and sometimes vomiting. Despite its name, it can occur at any time of day. This is due to hormonal changes, particularly the increase in human chorionic gonadotropin (hCG) and estrogen levels. While it can be uncomfortable, morning sickness is often considered a sign that the pregnancy is progressing normally.
2. Fatigue:
Many women experience overwhelming tiredness during the second month. The body is working hard to support the developing embryo, and hormonal fluctuations, particularly the rise in progesterone, can lead to increased drowsiness and fatigue. Rest is crucial, and it’s important to listen to your body’s needs.
3. Breast Tenderness:
Hormonal changes can make the breasts feel sore, swollen, or sensitive. This is a result of the body preparing for breastfeeding, with increased blood flow and changes in the breast tissue. Wearing a supportive bra and avoiding activities that might cause discomfort can help manage this symptom.
4. Uterus Expanding:
As the embryo grows, the uterus begins to expand to accommodate it. By the end of the second month, although still small, the uterus is starting to stretch. This can lead to sensations of cramping or mild abdominal discomfort, similar to menstrual cramps. However, if the cramps are severe or accompanied by bleeding, it’s important to consult a healthcare provider.
5. Changes in Skin, Hair, and Nails:
Pregnancy hormones can cause noticeable changes in the skin, hair, and nails. Some women may experience a “pregnancy glow,” characterized by more radiant skin due to increased blood circulation. However, others might notice changes like increased oiliness, acne, or darkening of the skin in certain areas (known as hyperpigmentation). Hair might become thicker or shinier, while nails may grow faster, but they might also become more brittle. It’s important to maintain a skincare routine that addresses these changes and consult a dermatologist if needed.
6. Frequent Urination:
As the uterus begins to grow, it can place pressure on the bladder, leading to an increased need to urinate. This is a common symptom during the second month and may become more noticeable as the pregnancy progresses.
7. Food Cravings and Aversions:
Hormonal changes can also lead to specific food cravings or aversions. Some women might find themselves suddenly craving certain foods they didn’t particularly enjoy before, while others might develop a strong dislike for foods they previously loved. These changes are usually temporary and vary widely from person to person.
8. Bloating and Gas:
Hormonal fluctuations, particularly the increase in progesterone, can cause the digestive system to slow down, leading to bloating and gas. This can result in a feeling of fullness or discomfort in the abdomen.
B. Emotional Changes:
1. Mood Swings:
Emotional fluctuations are common during the second month as hormones are in flux. Pregnant women may find themselves feeling more sensitive or experiencing rapid changes in mood. It’s important to acknowledge these feelings and communicate with loved ones for support. Practicing relaxation techniques such as deep breathing, yoga, or meditation can also help manage emotional changes.
2. Increased Anxiety or Worry:
The realization of being pregnant, coupled with the physical changes, can lead to heightened anxiety or worry. Concerns about the health of the baby, the progression of the pregnancy, or the future in general are common. Seeking reassurance from healthcare providers and discussing these feelings with a partner or support network can help manage these emotions.
3. Excitement and Joy:
Alongside anxiety, many women also experience feelings of excitement and joy as they begin to think about the future and the arrival of their baby. These positive emotions can fluctuate, but they play a significant role in the overall emotional experience during early pregnancy.
How Baby’s Development Takes Place in the Second Month:
A. Fetal Growth – Development of Major Organs and Systems:
1. Neural Tube Development:
The neural tube, which eventually becomes the baby’s brain, spinal cord, and central nervous system, starts forming early in the second month. Around week 6, this tube closes, and the brain begins to develop into three primary sections: the forebrain, midbrain, and hindbrain. Each of these sections will later form different parts of the brain responsible for various functions, such as thinking, movement, and basic survival functions.
2. Cardiovascular System:
The heart begins to beat around week 6, and by week 7, it starts to pump blood through the developing circulatory system. Although the heart is still forming its final structure, including the four chambers, it’s already working to circulate nutrients and oxygen to support the embryo’s rapid growth. This early heartbeat can sometimes be detected during an ultrasound by the end of the second month.
3. Digestive and Respiratory Systems:
The beginnings of the digestive system start to form, with the intestines and stomach starting to develop. Similarly, the respiratory system begins its initial stages, with the formation of structures that will eventually become the lungs. These systems are crucial for the baby’s survival after birth, even though they won’t fully function until later in the pregnancy.
4. Growth of the Embryo (Size Comparisons):
The embryo experiences rapid growth during the second month, doubling in size over these four weeks. By the end of week 8, the embryo is roughly the size of a raspberry, measuring about 0.5 to 0.8 inches (1.2 to 2 centimeters). Despite its small size, the embryo’s shape becomes more defined, with the head taking up a significant portion of the body, reflecting the rapid development of the brain. The growth at this stage is so significant that by the end of this month, the embryo starts to look more like a tiny human.
B. Key Milestones – Formation of the Brain, Heart, and Spinal Cord:
1. Brain Development:
As the neural tube closes, the brain begins to grow at an accelerated rate. The forebrain will eventually develop into the cerebral cortex, which is responsible for thinking, memory, and voluntary actions. The midbrain controls vision and hearing, while the hindbrain manages essential functions such as breathing and heart rate. Although the brain is still primitive, this foundational development is crucial for the baby’s overall neurological growth.
2. Heart Development:
The heart’s early formation is a critical milestone, as it starts to beat and pump blood through the embryo’s body. By the end of the second month, the heart has developed a basic structure, although it will continue to refine and grow throughout the pregnancy. The early heartbeat is a key sign of life and an important indicator of the embryo’s health.
3. Spinal Cord Development:
The spinal cord, formed from the neural tube, begins to elongate as the embryo grows. This cord will eventually connect the brain to the rest of the body, allowing for communication between the central nervous system and peripheral organs and muscles. The early development of the spinal cord sets the stage for the baby’s motor functions and sensory perception.
C. Development of Facial Features and Limb Buds:
1. Facial Features:
By the end of the second month, the embryo starts to show the early stages of facial development. Small indentations appear where the eyes and ears will form. The mouth and lower jaw begin to shape, and tiny nostrils start to develop. Although these features are still rudimentary, they represent the beginning of the facial structure that will continue to evolve over the coming months.
2. Limb Bud Development:
Limb buds appear as small protrusions from the sides of the embryo, marking the early stages of arm and leg development. These buds will gradually elongate and segment, forming the upper and lower limbs. While the fingers and toes are not yet distinct, the basic outlines of arms and legs are starting to take shape. This early development is crucial for the eventual formation of functional limbs.
3. Formation of Eyes and Ears:
The eye structures, including the optic vesicles, begin to form, although they are still covered by a thin layer of skin. The ear structures also start to develop, with the beginnings of the inner ear forming, which will later contribute to the sense of hearing and balance. These sensory organs are essential for the baby’s interaction with the world after birth.
How Prenatal Care can be Ensured:
A. Early Prenatal Visits:
Early prenatal visits are foundational for ensuring a healthy pregnancy and addressing any potential issues before they become serious. Here’s why they matter:
1. Confirmation of Pregnancy:
While home pregnancy tests are a good initial indicator, a visit to your healthcare provider provides a definitive confirmation. This is usually done through a blood test, which is more sensitive and can detect pregnancy earlier than urine tests. The doctor may also perform an initial physical examination.
2. Establishing Due Date:
Determining the precise due date is crucial for planning future care and monitoring fetal development. This is often done using your last menstrual period (LMP) and/or an early ultrasound. Accurate dating helps in scheduling further ultrasounds and screenings.
3. Health Risk Assessment:
Your healthcare provider will review your medical history to identify any potential risks or conditions that could affect your pregnancy. This includes chronic conditions like diabetes or hypertension, and any previous pregnancy complications. Early identification allows for tailored care strategies to mitigate these risks.
4. Educational Opportunity:
Early visits provide an opportunity to educate expectant parents on various aspects of pregnancy, childbirth, and parenting. This includes discussions on what to expect in each trimester, prenatal vitamins, and lifestyle changes.
B. First Ultrasound and What to Expect:
The first ultrasound, typically performed between 6-8 weeks, is a key milestone in early pregnancy care:
1. Confirming Viability:
The primary goal of this ultrasound is to confirm that the pregnancy is viable and located in the uterus. The presence of a heartbeat, visible as early as 6 weeks, is a reassuring sign that the pregnancy is progressing normally.
2. Determining Gestational Age:
By measuring the embryo or fetus from crown to rump (the CRL measurement), the ultrasound provides an accurate gestational age, which refines the estimated due date. This is crucial for tracking fetal growth and development.
3. Identifying Multiple Pregnancies:
The ultrasound can reveal whether you are carrying multiples (twins, triplets, etc.). This is important for managing prenatal care, as multiple pregnancies often come with increased risks and require specialized monitoring.
4. Assessing Early Development:
Early ultrasounds can detect certain anomalies or issues, such as abnormal growth patterns or the presence of certain conditions. While not all conditions are detectable, it provides an early overview of the fetus’s health.
C. What to Expect During the Ultrasound:
1. Procedure:
For a transabdominal ultrasound, you’ll lie on an exam table while a gel is applied to your abdomen. A transducer is then moved over your belly to capture images. For an early pregnancy, a transvaginal ultrasound might be used, involving a small probe inserted into the vagina for clearer images.
2. Duration:
The procedure usually lasts between 15 and 30 minutes, depending on the clarity of images and any additional measurements needed.
3. Experience:
You might feel some mild discomfort, especially with a transvaginal ultrasound, but it is generally not painful. You’ll be able to see the images on a monitor, which can be an exciting and reassuring experience.
D. Blood Tests and Screenings
Blood tests and screenings in the second month of pregnancy are essential for assessing maternal and fetal health:
1. Blood Type and Rh Factor:
Your blood type (A, B, AB, O) and Rh factor (positive or negative) are tested. This is important for managing potential Rh incompatibility, which can cause problems in the baby if not addressed.
2. Complete Blood Count (CBC):
A CBC checks for anemia, which is common in pregnancy and can lead to fatigue and other issues. It also helps in detecting infections or other blood disorders that might affect your pregnancy.
3. Hormone Levels:
Levels of hormones like hCG (human chorionic gonadotropin) and progesterone are measured. These hormones support pregnancy and their levels can provide insights into the health of the pregnancy.
4. Infectious Disease Screening:
Tests for diseases such as hepatitis B, syphilis, and HIV are conducted. Detecting these early allows for treatment that prevents transmission to the baby and ensures appropriate care.
5. Genetic Screening:
Depending on your risk factors and family history, your healthcare provider may recommend genetic screenings to assess the risk of chromosomal abnormalities, such as Down syndrome. These screenings can involve blood tests and sometimes ultrasounds.
What shall be the Proper Nutrition and Diet:
A. Essential Nutrients:
1. Folic Acid:
Crucial for preventing neural tube defects such as spina bifida. A daily intake of 400-800 micrograms is recommended. Sources include leafy green vegetables, fortified cereals, and prenatal vitamins. (Though, the doctor’s recommendation would be the best)
2. Iron:
Necessary for the production of hemoglobin, which carries oxygen in the blood. During pregnancy, your blood volume increases, so you need more iron. Aim for 27 milligrams daily, found in red meat, poultry, fish, lentils, and fortified cereals. (Though, the doctor’s recommendation would be the best)
3. Calcium:
Supports the development of the baby’s bones and teeth. If your intake is inadequate, the baby will draw calcium from your bones, which can weaken them. Aim for 1,000 milligrams daily through dairy products, fortified plant-based milks, and leafy greens. (Though, the doctor’s recommendation would be the best)
B. Foods to Eat and Avoid:
1. Foods to Eat:
Fruits and Vegetables: Rich in vitamins, minerals, and fiber. Aim for a variety of colors to ensure a broad range of nutrients.
Whole Grains: Brown rice, whole wheat bread, and oats provide essential nutrients and fiber.
Lean Proteins: Important for tissue growth. Include chicken, turkey, tofu, beans, and fish low in mercury.
Dairy Products: Provide calcium and protein. Opt for low-fat options if preferred.
2. Foods to Avoid:
Raw or Undercooked Seafood, Meat, and Eggs: Risk of foodborne illnesses like salmonella and listeria, which can harm both mother and baby.
Unpasteurized Dairy Products: Can carry harmful bacteria such as listeria.
High-Mercury Fish: Fish like shark, swordfish, and king mackerel contain high levels of mercury, which can affect the baby’s brain development.
Caffeine and Alcohol: Excessive caffeine can increase the risk of miscarriage, and alcohol can cause fetal alcohol spectrum disorders. Limit caffeine to 200 milligrams per day and avoid alcohol completely.
Lifestyle Adjustment Requirements:
A. Recommendations for Exercise and Rest:
1. Exercise:
Engaging in moderate exercise can help manage weight gain, boost mood, and improve sleep. Safe activities include brisk walking, swimming, and prenatal yoga. Avoid high-impact exercises or activities with a risk of falling.
2. Rest:
Your body is working hard to support the pregnancy, so adequate rest is essential. Aim for 7-9 hours of sleep per night. Listen to your body and take naps if you feel fatigued. Creating a relaxing bedtime routine can help improve sleep quality.
B. Managing Stress and Mental Health:
1. Stress Management:
High levels of stress can negatively impact both you and your baby. Incorporate relaxation techniques into your daily routine, such as deep breathing exercises, prenatal massage, or gentle stretching. Maintaining a support network of family and friends can also help.
2. Mental Health:
Pregnancy can bring a whirlwind of emotions. It’s important to communicate openly with your partner, friends, or a therapist about your feelings. If you experience severe anxiety or depression, seek help from a mental health professional. Many providers offer counseling specifically tailored to pregnant women.
Common Concerns and Questions:
1. Spotting:
A. When It’s Normal:
Implantation Bleeding: Light spotting can occur when the fertilized egg implants itself into the uterine lining. This usually happens around 6-12 days after conception and can be mistaken for a light period. Implantation bleeding is typically light pink or brown and lasts for a few hours to a couple of days.
Cervical Changes: Increased blood flow to the cervix can cause light spotting, especially after a Pap smear or vaginal exam. This is generally harmless.
B. When to Call a Doctor:
Heavy Bleeding: If you experience bleeding that is heavier than a light period, or if the bleeding is accompanied by clots, it could be a sign of a more serious condition, such as a miscarriage or an ectopic pregnancy.
Persistent Spotting: If spotting continues beyond a couple of days or is accompanied by severe cramping, it’s important to consult a healthcare provider.
Associated Symptoms: If spotting is accompanied by severe pain, dizziness, or shoulder pain, it could indicate an ectopic pregnancy, which requires immediate medical attention.
2. Cramping:
A. When It’s Normal:
Implantation Cramping: Mild cramping can occur as the embryo implants into the uterine wall. This is usually mild and similar to menstrual cramps.
Uterine Growth: As the uterus expands to accommodate the growing embryo, you may experience mild cramping or stretching sensations. This is generally harmless and part of normal pregnancy changes.
B. When to Call a Doctor:
Severe Cramping: Intense cramping, particularly if it is one-sided or accompanied by bleeding, may be a sign of an ectopic pregnancy or miscarriage.
Persistent Pain: Continuous or worsening cramping, especially if it interferes with daily activities or is accompanied by other concerning symptoms like fever or bleeding, should be evaluated by a healthcare provider.
Pain with Fever or Nausea: If cramping is accompanied by fever, nausea, or vomiting, it could indicate an infection or other complications.
3. Weight Gain:
A. What’s Typical and Healthy:
General Guidelines: In the second month of pregnancy, weight gain is typically minimal. Most women gain about 1-4 pounds in the first trimester. This can vary based on pre-pregnancy weight, overall health, and individual factors.
B. Healthy Weight Gain:
Pre-Pregnancy Weight: Weight gain recommendations can vary based on your pre-pregnancy weight. Women with a normal BMI (18.5-24.9) are generally advised to gain 25-35 pounds throughout pregnancy. Those who are underweight might need to gain more, while those who are overweight or obese might be advised to gain less.
Balanced Diet: Focus on a balanced diet rich in essential nutrients, including proteins, vitamins, and minerals. Ensure adequate intake of fruits, vegetables, whole grains, and lean proteins.
Hydration: Staying hydrated is crucial. Aim to drink at least 8-10 glasses of water daily, or more if needed based on activity level and environmental conditions.
C. Managing Weight:
Avoiding Excessive Weight Gain: Excessive weight gain can lead to complications such as gestational diabetes and hypertension. Monitor your weight regularly and discuss any concerns with your healthcare provider.
Regular Check-Ups: Regular prenatal visits will monitor your weight and overall health. Your healthcare provider will offer guidance if your weight gain is outside the typical range.
4. Sex During Pregnancy:
A. When It’s Generally Safe:
Healthy Pregnancy: For most women with a healthy pregnancy, sex is safe throughout the pregnancy. The baby is well-protected by the amniotic sac and uterus, and sex will not harm the baby.
Comfort and Desire: Sexual activity should be based on comfort and mutual desire. Many couples continue to have a satisfying sex life during pregnancy.
B. When to Exercise Caution:
High-Risk Pregnancy: If you have a high-risk pregnancy or have been advised to avoid sex by your healthcare provider due to conditions like placenta previa, preterm labor risk, or other complications, it’s important to follow their guidance.
Symptoms to Watch For: If you experience any unusual symptoms after sex, such as bleeding, cramping, or increased discharge, consult your healthcare provider.
Position Adjustments: As your pregnancy progresses, certain positions may become uncomfortable. Experiment with different positions that are comfortable for both partners.
5. Emotional and Physical Considerations:
Body Changes: Pregnancy brings many physical changes, and it’s normal for body image and sexual desire to fluctuate. Open communication with your partner is key.
Comfort and Intimacy: Focus on maintaining intimacy and connection with your partner. Non-sexual forms of affection, such as cuddling and gentle touches, can also help maintain a strong relationship.
Planning Ahead to the Next Step:
The Third Month of Pregnancy:
By planning ahead and preparing for the upcoming changes in the third month of pregnancy and beyond, you can navigate the transition into the second trimester with greater confidence and ease, ensuring both you and your baby are well-supported.
A. What to Expect in the Upcoming Weeks:
1. Fetal Development:
Size and Growth: By the end of the third month, the fetus is about 2-4 inches long and weighs around 0.5-1 ounce. It is rapidly growing, with major organs and systems developing.
Movement: The fetus may start to make small movements, although they are not usually felt by the mother yet. The fetus will begin to develop distinct features, including fingers and toes, and may even start making reflex movements.
Development Milestones: Key developments include the formation of facial features, limbs, and the beginning of more complex brain development. The baby’s heart is fully formed and beating strongly.
2. Maternal Changes:
Physical Symptoms: You may experience a reduction in nausea and fatigue as you move into the second trimester. Energy levels might start to improve, and you may notice a decrease in the severity of early pregnancy symptoms.
Body Changes: Your uterus continues to grow, and your body will start showing signs of pregnancy more prominently. You might begin to develop a small baby bump as your uterus expands.
3. Prenatal Care:
Ultrasound: You will likely have a detailed ultrasound around 11-14 weeks (nuchal translucency scan) to check for any early signs of chromosomal abnormalities and to get a clearer picture of the baby’s development.
Screenings: You may also undergo additional blood tests and screenings to assess the risk of genetic disorders and to check for any new health concerns.
B. Preparing for Further Changes:
1. Managing Symptoms:
Morning Sickness: If you’re still experiencing nausea, continue with strategies like eating small, frequent meals, staying hydrated, and avoiding strong odors. Ginger and vitamin B6 supplements may also help alleviate symptoms.
Fatigue: As energy levels start to improve, balance rest with light physical activity. Ensure you’re getting adequate sleep and listen to your body’s needs.
2. Diet and Nutrition:
Balanced Diet: Continue focusing on a balanced diet rich in essential nutrients. As your appetite may change, prioritize nutrient-dense foods and avoid empty-calorie snacks.
Hydration: Maintain proper hydration by drinking plenty of water. This helps with digestion, prevents constipation, and supports overall health.
3. Comfort Measures:
Clothing: As your body changes, you may need to start wearing maternity clothes that accommodate your growing belly. Choose comfortable, breathable fabrics to stay cool and comfortable.
Exercise: Engage in moderate exercise such as walking, swimming, or prenatal yoga to boost energy levels, improve mood, and support overall health. Avoid high-impact or strenuous activities that could cause discomfort.
C. Tips for Involving Your Partner or Family:
1. Communication:
Open Dialogue: Keep the lines of communication open with your partner about your feelings, concerns, and experiences. Sharing your thoughts helps in managing expectations and maintaining a supportive relationship.
Participation: Encourage your partner to attend prenatal appointments with you. This involvement helps them feel more connected and informed about the pregnancy.
2. Education and Preparation:
Prenatal Classes: Consider enrolling in prenatal classes together. These classes provide valuable information about childbirth, breastfeeding, and newborn care, and can be a bonding experience for both partners.
Preparing for Baby: Start discussing and planning for practical aspects, such as creating a baby registry, setting up a nursery, and deciding on parenting roles and responsibilities.
3. Family Support:
Involve Family Members: Share your pregnancy journey with close family members. Their support can be invaluable, and they may offer practical help or emotional support as you prepare for the baby’s arrival.
Discuss Plans: Talk with family about any changes in routines, such as additional support needed or adjustments in household responsibilities. Ensuring everyone is on the same page helps in managing the transition smoothly.
4. Self-Care:
Relaxation: Make time for self-care and relaxation. Engage in activities that you enjoy and that help you unwind, such as reading, taking baths, or practicing mindfulness.
Support Networks: Connect with other expectant mothers through support groups or online forums. Sharing experiences and advice can be reassuring and provide additional support.
The Final Thoughts:
In the second month of pregnancy, it’s important to remember that each woman’s experience can differ significantly. Symptoms such as mild cramping, spotting, and fatigue are common and vary widely from person to person. It’s normal to have different experiences, but if you notice any unusual or severe symptoms, such as heavy bleeding or intense pain, it’s crucial to seek medical advice.
Prioritizing self-care remains essential. Ensure you’re eating a balanced diet, staying hydrated, and getting plenty of rest. These practices help manage early pregnancy symptoms and support your overall well-being. Following your healthcare provider’s recommendations for prenatal vitamins and attending regular check-ups will further ensure both your health and the health of your baby.
Open communication with your healthcare provider is key. Discuss any concerns or changes you’re experiencing, and don’t hesitate to ask questions about your pregnancy. Staying informed and having regular discussions with your provider will help you navigate this early stage with confidence and peace of mind.
Courtesy Image: FreePik

